Considering a jaw bone implant? A jaw bone implant is a dental implant that relies on healthy jaw bone to fuse with the implant post. Jaw bone quality matters because bone volume and density determine whether an implant will be stable long term. This article explains what a jaw bone implant is, who makes a good candidate, how dentists evaluate jaw bone, treatment options when bone is limited, and practical next steps for a personalized evaluation.
If you’re wondering whether a jaw bone implant Austin, TX evaluation is right for you, this guide will walk you through common procedures, recovery expectations, and when advanced solutions like zygomatic or All‑on‑X implants are recommended.
What Is a Jaw Bone Implant?
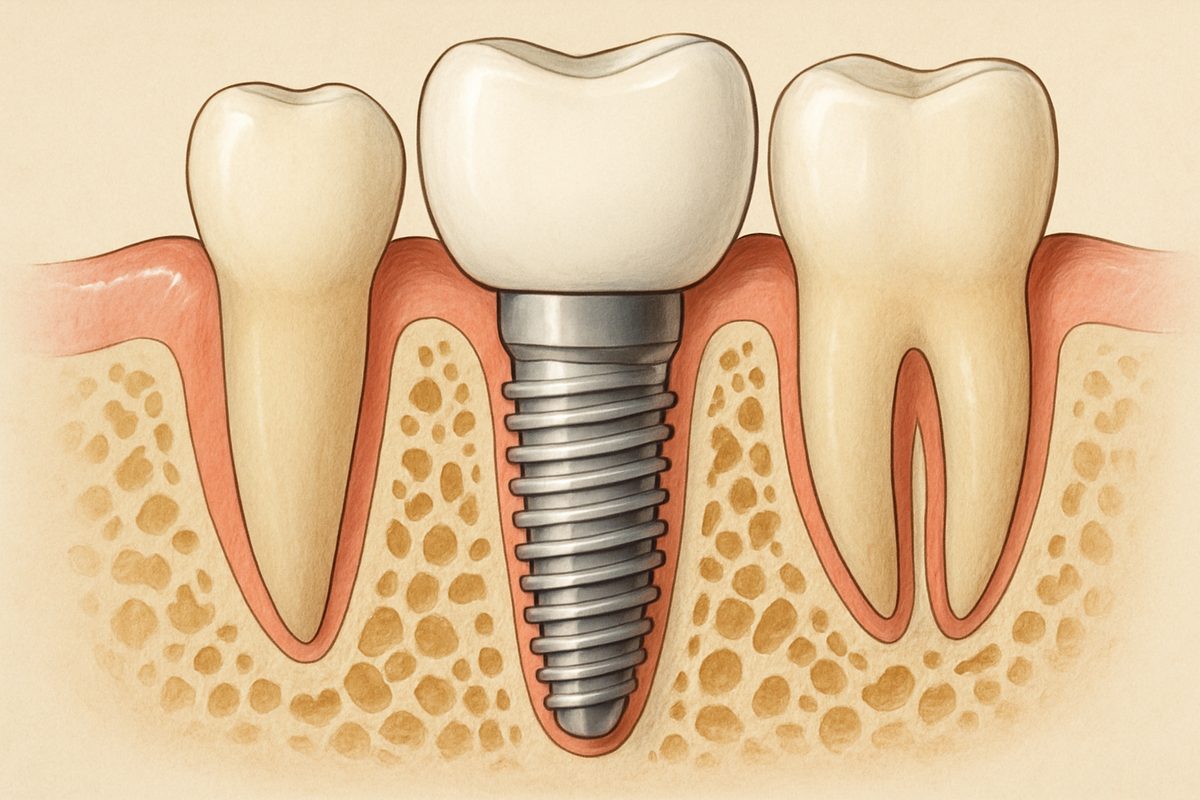
A jaw bone implant is a titanium or titanium‑alloy post placed into the jaw to replace a missing tooth root. Over weeks to months the bone grows around the post in a process called osseointegration. Once stable, the implant supports a crown, bridge, or full‑arch prosthesis.
Standard implants work when there is enough jaw bone. When bone is thin or low, dentists may use bone grafting to add volume. For severe bone loss, alternative approaches include zygomatic implants (anchored in the cheekbone) or pterygoid implants (anchored toward the back of the upper jaw). These solutions let patients receive implants without extensive grafting.
Who Makes a Good Candidate for a Jaw Bone Implant?
Ideal candidates
Good candidates for a jaw bone implant are healthy adults who:
- Keep good oral hygiene
- Have controlled medical conditions (like managed diabetes)
- Have enough jaw bone or are willing to consider grafting or advanced implant options
When you might not be a candidate
Some conditions raise risk or delay treatment. These include active smoking, uncontrolled diabetes, recent head/neck radiation, and severe periodontal disease. In many cases these issues can be managed so a patient becomes eligible later—for example, quitting smoking, treating gum disease, or stabilizing medical conditions.
Special candidacy: severe bone loss
For people with major jaw bone loss, a traditional implant plus graft may not be best. Options include:
- Zygomatic implants or pterygoid implants that anchor in stronger bone outside the jaw
- All‑on‑X full‑arch restorations that use several implants to support a prosthetic arch
These techniques often avoid long grafting timelines and can restore function faster.
How Dentists Determine Candidacy for a Jaw Bone Implant
Evaluation starts with medical and dental history, a clinical exam, and an oral hygiene check. The most important test is a CBCT 3D scan. A CBCT shows bone volume, density, sinus and nerve locations, and helps plan exact implant positions using digital software.
Digital planning allows a dentist to measure bone and choose the correct implant size, angle, and whether grafting or alternative implants are needed. This is why 3D imaging is standard for jaw bone implant planning.
Common Procedures to Make You a Candidate
Bone grafting and sinus lifts
Bone grafts add volume where bone is thin. Grafts use your own bone, donor bone, or synthetic materials. Sinus lifts raise the sinus floor to create space for bone in the upper back jaw. Healing typically takes several months before placing the implant.
Platelet Rich Plasma (PRP) and healing support
PRP uses growth factors from your blood to speed healing and reduce recovery time. When used with grafts or implants, PRP may improve bone formation and soft tissue healing.
Advanced implant solutions
Guided surgery uses digital guides for precise implant placement. For low jaw bone cases, zygomatic and pterygoid implants or All‑on‑X restorations provide stable support without extensive grafting. These advanced options expand candidacy for patients who once had few choices.
Recovery, Risks, and Success Rates
After implant placement expect swelling, mild pain, and light bleeding for a few days. Osseointegration takes 3–6 months for most people. Risks include infection, implant failure, nerve or sinus issues, and graft complications. Success rates are high—often above 90%—when patients maintain good oral care and manage health conditions.
Long‑term success depends on bone quality, oral hygiene, smoking status, and overall health. Regular dental visits and cleanings are essential to protect your investment.
Why Choose a Specialist for Jaw Bone Implant Care
Complex bone cases benefit from a specialist. Union Dental Implant Center focuses exclusively on advanced implant dentistry. Led by Dr. Adam Carter, the center combines CBCT 3D imaging, computer‑guided surgery, and an on‑site digital lab to plan and deliver precise results. Their in‑house tools—3D printing, CAD/CAM milling, and PRP—help treat difficult jaw bone situations, including zygomatic and pterygoid solutions, with fewer referrals and faster timelines.
Next Steps: Am I a Candidate?
Common questions patients ask:
- How do I get evaluated? — Schedule a consult with CBCT 3D imaging and a clinical exam.
- How long does it take to know? — Many practices can give a treatment plan after one visit with 3D scans; full planning may take a few days.
- Will insurance cover it? — Ask about insurance, financing, and phased treatment to fit budgets.
If you want a personalized assessment for a jaw bone implant Austin, TX, schedule a consultation to review your 3D scan, discuss grafting or advanced implant options, and get a clear treatment timeline. A specialist can explain which path—grafting, zygomatic/pterygoid implants, or All‑on‑X—is best for your anatomy and goals.
Ready to learn if you’re a candidate for a jaw bone implant Austin, TX? Book a consultation for a full exam and CBCT review to get a clear, personalized plan.